Ever since insulin was first used in Toronto 100 years ago, the daily lives of people living with type 1 diabetes (T1D) have been transformed by many discoveries.
Thanks to the formulation of insulin as a treatment for type 1 diabetes, this short-term fatal illness was transformed into a chronic one. The discovery was just the starting point for many innovations to come. Ever since the first injection of insulin was administered to Leonard Thompson on January 11, 1922, the daily lives of people with T1D have significantly improved—and hopefully, it will keep on getting better.
Insulin as a starting point
Insulin can only treat diabetes; it cannot cure it. Its formulation evolved very quickly—from animal insulin (taken from the pancreases of pigs or cows) to man-made, or “human” insulin. More recently, insulin analogs have helped to make treatment more flexible with varying durations of action, which can reduce the risk of hypoglycemia most of the time.
Over the past few years, new formulations have become available with modes of action that aim to imitate as closely as possible the way the pancreas naturally secretes insulin. The most recent ones include longer-acting insulin (e.g., Tresiba®, Toujeo®) that lasts 30–42 hours and ultra-rapid insulin (e.g., Fiasp®) that starts acting 4–7 minutes after the injection. These new types of insulin provide more flexibility in injection timing and offer a wider range of treatment options.
New technology is also constantly available to help reduce the burden of diabetes management and improve glycemic control.
Below is a summary of tools available in Quebec that can help—in most cases—to improve blood sugar management.
Continuous glucose monitoring systems

Continuous glucose monitoring (CGM) systems are one of the greatest innovations from the past few years. CGM technology allows the user to view their blood sugar trends in real time and over a period of time. The first CGM system on the Canadian market was approved by Health Canada in 2014. Four devices are currently available—FreeStyle Libre, FreeStyle Libre 2, Dexcom G6 and Guardian—two of which are covered by the RAMQ under certain criteria (FreeStyle Libre and Dexcom G6, since May 25).
CGMs work with a sensor that is attached to the skin—a very fine sensor wire is inserted underneath the skin—for six to fourteen days, depending on the device. CGMs reduce or even eliminate the need for finger pricks and provide a detailed view of blood sugar levels all day and all night long.
Trend arrows help to predict where blood sugar levels will be in the next few minutes, and some systems will sound alerts depending on blood sugar levels to avoid or start treating hypoglycemia or hyperglycemia.
The efficacy of CGMs in reducing hypoglycemia, improving glycemic control over time (e.g., HbA1c levels) and improving quality of life has been confirmed by many studies.
According to the BETTER registry’s preliminary data, approximately 70% of adults and children with T1D in Quebec use a CGM system.
Insulin pumps

Insulin pumps have been available in Quebec since the 1980s. These devices administer rapid-acting insulin subcutaneously in microdoses throughout the day and night (basal rate) and boluses (e.g., at mealtimes).
The insulin is administered this way to mimic how the pancreas naturally secretes insulin, but this method still requires user interventions and adjustments, as well as several blood sugar measurements per day.
In most cases, insulin pumps help to improve blood sugar management, but their cost and the need to carry them continuously are prohibitive. In Quebec, the Insulin Pump Access Program covers the cost of insulin pumps for patients who start using the pump before they turn 18 years old.
According to the BETTER registry’s preliminary data, approximately 40% of adults and children with T1D in Quebec use an insulin pump.
Hybrid closed loop systems

Hybrid closed loop systems, also known as artificial pancreases, take us one step closer to the automation of insulin pumps. Quebec authorized a first hybrid closed loop system in 2018, and there are currently three systems available: Medtronic 670G, Medtronic 770G and Tandem Control-IQ.
These systems work with an insulin pump and a paired CGM. An algorithm automatically adjusts the basal rate according to blood sugar readings.
Although they are also called “artificial pancreases,” user interventions are still required for meal and correction boluses, for treating hypoglycemia and for situations where blood sugar levels fluctuate very quickly (e.g., during physical activity).
The RAMQ does not cover any of the hybrid closed loop systems, but many private insurance plans do cover the system components.
Many studies have found that hybrid closed loop systems help to increase time spent in range (between 4 and 10 mmol/L) while offering the same benefits as CGMs (fewer hypoglycemic episodes, better quality of life, etc.). They also simplify many aspects of type 1 diabetes management.
What about the future?
Continuous ketone monitoring devices, islet transplantation, fully automated insulin pumps, use of drugs typically reserved for treating type 2 diabetes… the future looks bright, and research is ongoing. But the main objective remains to find a cure.
Researchers are currently looking at two avenues to achieve this: 1. Finding a way to repel the immune system’s continuous attack on insulin-producing beta cells either by stopping it or by protecting the new beta cells (encapsulation); 2. Finding a way to restore the body’s ability to produce its own insulin either by regenerating the remaining cells or by transplanting healthy cells from animals.
While new treatments and technology often improve the daily lives of people with type 1 diabetes, they are expensive, and most are not covered by the RAMQ. Some people are able to afford them thanks to a private insurance plan, but according to preliminary data from the BETTER registry, 21% of people with T1D rely on RAMQ coverage only.
Let’s continue our work and make things happen!
If you or your child live with type 1 diabetes in Quebec, consider helping us to make things happen by signing up for the BETTER registry (a kind of census).
Filling out the questionnaire and completing your registration should take between 15 and 30 minutes.
You will be able to participate in the webinars that we organize.
Please note: Those webinars will be given in French but question could be asked and answered in English.
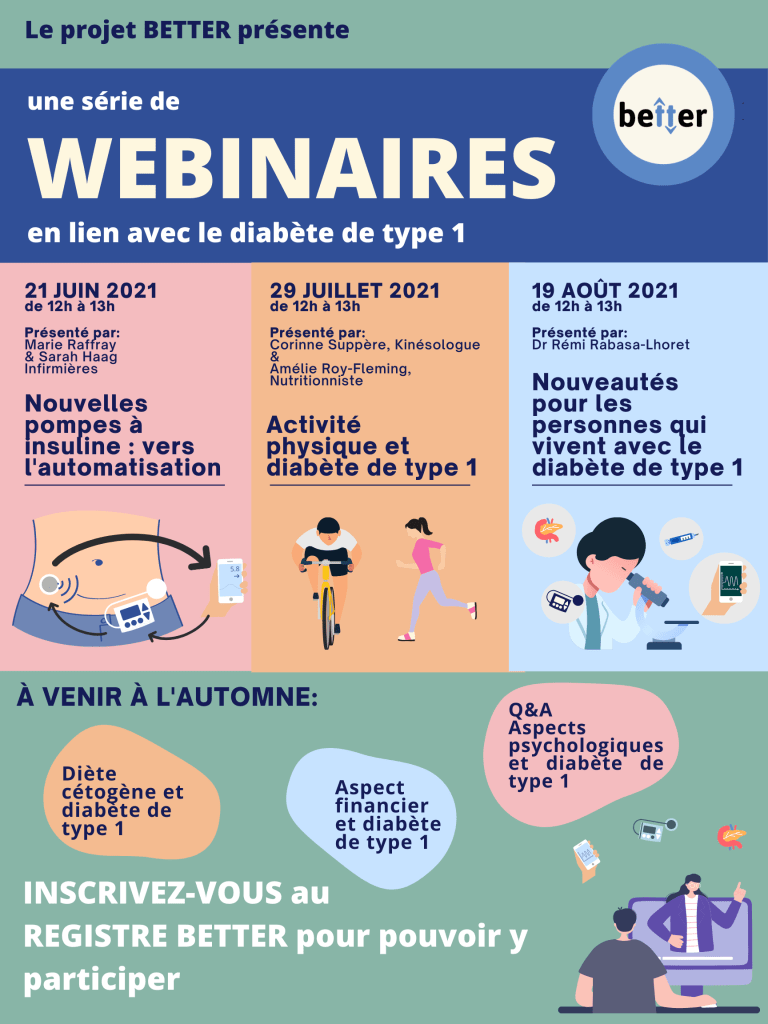

The next one will be held on June 21st and will focus on the new insulin pumps (hybrid closed loop systems).
We will tell you all about how they work, the advantages, the cost, etc.
Participate in the BETTER registry!

First registry of people living with T1D in Canada.
Learn More



2 thoughts on “Type 1 Diabetes: 100 Years of Research and Tech Innovation”
Comments are closed.