People with type 1 diabetes (T1D) who use a continuous glucose monitoring (CGM) system (e.g., Dexcom, FreeStyle Libre) and/or an insulin pump (e.g., Medtronic, Omnipod) already know about some of the demoralizing problems they can experience with their devices.
For instance, problems can occur when:
- the device (sensor, catheter or pod) is ripped out against a door frame or handle;
- the device peels up (e.g., with sweat) and falls off before the end of its useful life;
- the adhesive under the device triggers an allergic skin reaction;
- the adhesive under the device leaves residue on the skin.
In summer, your device may tend to fall off your skin due to more abundant sweating and more frequent swimming. With these negative experiences, your desire to continue using these technologies can start to wane. But there’s no need to spend the whole summer in air-conditioned spaces or to avoid going for a swim!
For some people, the problem is not their device falling off, but rather redness, itching or a sensation of heat in the area where it’s placed. These allergic reactions can happen at any time, even with sensors that haven’t just been inserted. They can sometimes manifest after several days, weeks or even months of use.
Here are some possible solutions for reducing or resolving these issues, so you can have peace of mind and enjoy all the activities you want to do.
Poor adherence
Depending on your skin type or external factors (e.g., heavy sweating, physical activity), your sensor may be prone to falling off.
Luckily, there are different products that can help improve adherence.
These products can be used before or after you install the device.
- BEFORE
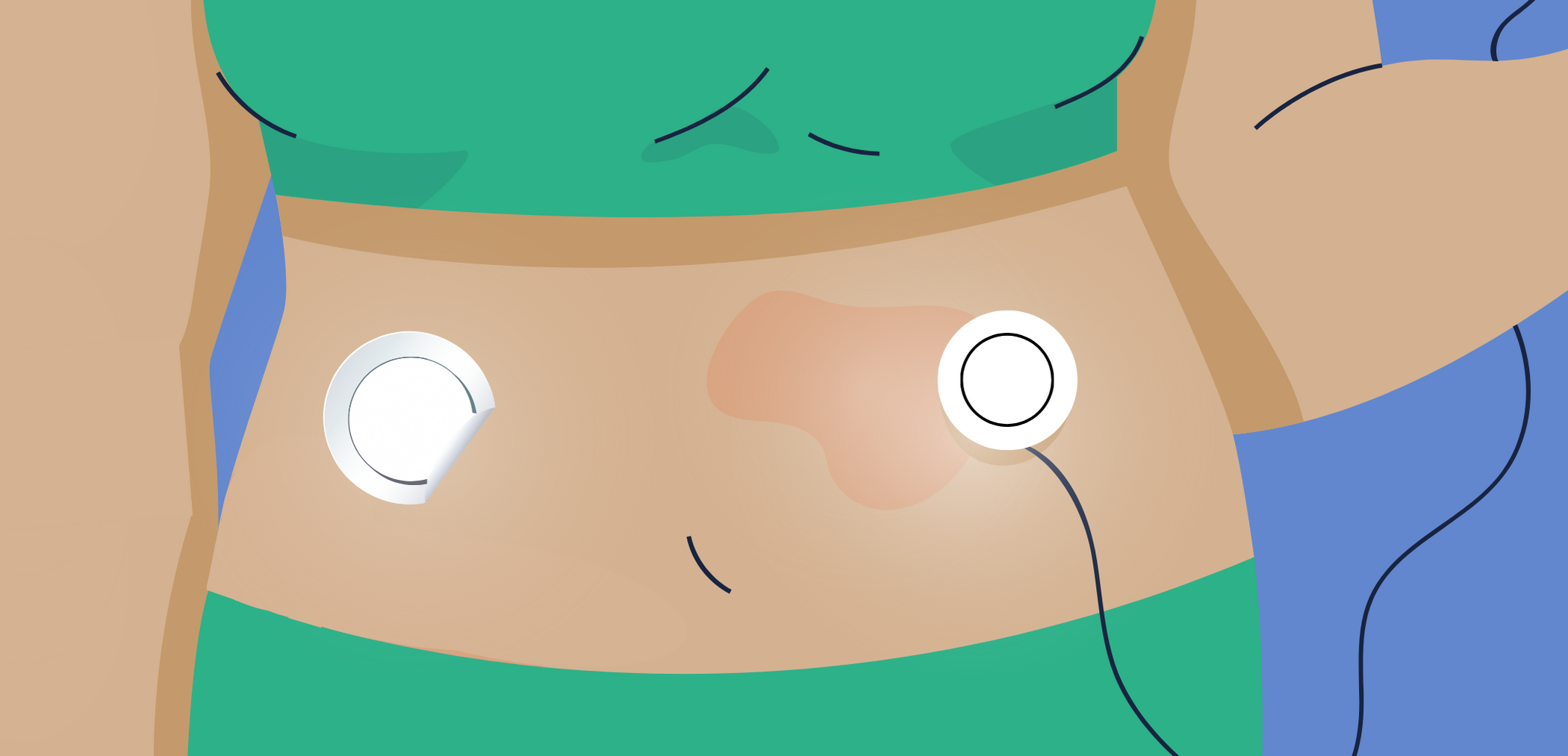
Certain products (e.g., Skin Tac™ wipe, Hollister® Adapt™ spray) or dressings (e.g., Tegaderm™, IV 3000◊, Hypafix®) can be applied on clean skin to help your sensor stick better to your skin.. In the case of dressings, it’s important to note that a small hole must be made beforehand to let the wire or cannula through and prevent it from bending during insertion.
- AFTER
The above-mentioned dressings can also be applied over the catheter or pod (insulin), and sometimes over the sensor/transmitter of your continuous glucose monitor, for better skin adherence. Note, however, that the Dexcom CGM cannot be covered up because this could affect their ability to transmit data. In that case, you need to make a hole in the dressing so that it doesn’t cover the sensor, but merely strengthens the adhesive.
Some sites also offer esthetic dressings that are adapted to the type of sensor that you wear (e.g., pumppeelz, pimpmydiabetes).
There are also armbands or other types of bands that you can put over the sensor (except for Dexcom) to help keep it in place, for instance during physical activity. The infusion site for your catheter or pod is also important and can be chosen based on your activities (e.g., swimming) or the clothes you’re wearing (e.g., do not insert it on the beltline).
Find out more in this list of products that we compiled.
Skin reactions
Some people can experience skin irritation or even an allergic reaction that is caused by the sticky portion of the sensor. Redness, a sensation of heat or itching can be experienced over and sometimes around the area where the sensor was inserted. This generally occurs even when the insertion site of the device is changed.
These reactions are generally caused by the glue used under the device. So, you may be able to solve this problem by switching to a different version (e.g., FreeStyle Libre 1 or Libre 2) or a different company.
Just like for adherence problems, there are products or dressings that can help to reduce these skin reactions.
You can try applying a protective skin barrier (e.g., Skin Prep◊, Cavilon™, Skin Tac™). These products form a barrier between the skin and the adhesive to reduce irritation.
There are also dressings (e.g., Tegaderm™, IV 3000◊, Hypafix®) that you can apply to the skin before you insert a device, in order to create a physical barrier on the skin. In the case of certain dressings, you’ll first need to make a small hole to let the wire or cannula through and prevent it from bending during insertion.
There are other prescription or over-the-counter products that help to decrease local skin inflammation. They’re applied before insertion. However, note that because some devices can remain in place for 6 to 14 days (e.g., sensors), the product’s effect can decrease, and skin reactions may return before you remove the sensor.
Find out more in this list of products that we compiled.
You may also want to try different insertion sites to see whether some areas of your body are less prone to reactions (e.g., reaction when the sensor is on the arm, but not on the abdomen).
If the allergy persists despite these different strategies, you’ll need to discuss this with your healthcare team to assess different solutions. A consultation with a dermatologist may be suggested in certain cases.
Glue residue
If you’re having a hard time removing your catheter or pod, or if there is glue residue on your skin, there are products that can help you remove them (e.g., Remove◊). Baby oil can also help to remove adhesive on the skin.
There are many products to help prevent your device from falling off, treat allergies or remove glue residue, and avoid any possible negative experiences. These solutions can vary depending on your skin type. Try the different available options to discover what works for you.
Participate in the BETTER registry!

First registry of people living with T1D in Canada.
Learn More